天路客按:“《论语·卫灵公》有言曰:“工欲善其事,必先利其器。居是邦也,事其大夫之贤者,友其士之仁者。”作为中国人相比都耳熟能详,这话的意思是要做好工作,先要使工具锋利。小说里面也有这话,如:“工欲善其事,必先利其器。今既一无所有,纵使大禹重生,亦当束手。”(清·李汝珍《镜花缘》第三十六回)。”(见天路客《现代方法学的进步终会打破中医残梦——兼谈中医缺少证伪能力》XYS20091104),科学有效的方法固然重要,但也不要迷信,惟方法论,任何方法学(Methodology)都是有局限的,都不是绝对的,不能唯方法论,否则科学方法更会使人迷失,一个清醒的人要避免被方法所掌握,即使RCT也远非万能,特转载此文以作说明,有兴趣者可以继续讨论。
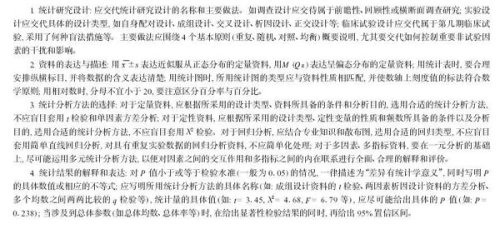
文章来源:BMJ 2003;327:1459-1461 (20 December), doi:10.1136/bmj.327.7429.1459
Hazardous journey
Parachute use to prevent death and major trauma related to gravitational challenge: systematic review of randomised controlled trials
Gordon C S Smith, professor1, Jill P Pell, consultant2
1 Department of Obstetrics and Gynaecology, Cambridge University, Cambridge CB2 2QQ, 2 Department of Public Health, Greater Glasgow NHS Board, Glasgow G3 8YU
Abstract
Objectives To determine whether parachutes are effective in preventing major trauma related to gravitational challenge.
Design Systematic review of randomised controlled trials.
Data sources: Medline, Web of Science, Embase, and the Cochrane Library databases; appropriate internet sites and citation lists.
Study selection: Studies showing the effects of using a parachute during free fall.
Main outcome measure Death or major trauma, defined as an injury severity score > 15.
Results We were unable to identify any randomised controlled trials of parachute intervention.
Conclusions As with many interventions intended to prevent ill health, the effectiveness of parachutes has not been subjected to rigorous evaluation by using randomised controlled trials. Advocates of evidence based medicine have criticised the adoption of interventions evaluated by using only observational data. We think that everyone might benefit if the most radical protagonists of evidence based medicine organised and participated in a double blind, randomised, placebo controlled, crossover trial of the parachute.
Introduction
The parachute is used in recreational, voluntary sector, and military settings to reduce the risk of orthopaedic, head, and soft tissue injury after gravitational challenge, typically in the context of jumping from an aircraft. The perception that parachutes are a successful intervention is based largely on anecdotal evidence. Observational data have shown that their use is associated with morbidity and mortality, due to both failure of the intervention1 2 and iatrogenic complications.3 In addition, “natural history” studies of free fall indicate that failure to take or deploy a parachute does not inevitably result in an adverse outcome.4 We therefore undertook a systematic review of randomised controlled trials of parachutes.
Methods
Literature search
We conducted the review in accordance with the QUOROM (quality of reporting of meta-analyses) guidelines.5 We searched for randomised controlled trials of parachute use on Medline, Web of Science, Embase, the Cochrane Library, appropriate internet sites, and citation lists. Search words employed were “parachute” and “trial.” We imposed no language restriction and included any studies that entailed jumping from a height greater than 100 metres. The accepted intervention was a fabric device, secured by strings to a harness worn by the participant and released (either automatically or manually) during free fall with the purpose of limiting the rate of descent. We excluded studies that had no control group.
Definition of outcomes
The major outcomes studied were death or major trauma, defined as an injury severity score greater than 15.6
Meta-analysis
Our statistical apprach was to assess outcomes in parachute and control groups by odds ratios and quantified the precision of estimates by 95% confidence intervals. We chose the Mantel-Haenszel test to assess heterogeneity, and sensitivity and subgroup analyses and fixed effects weighted regression techniques to explore causes of heterogeneity. We selected a funnel plot to assess publication bias visually and Egger’s and Begg’s tests to test it quantitatively. Stata software, version 7.0, was the tool for all statistical analyses.
Results
Our search strategy did not find any randomised controlled trials of the parachute.
Discussion
Evidence based pride and observational prejudice
It is a truth universally acknowledged that a medical intervention justified by observational data must be in want of verification through a randomised controlled trial. Observational studies have been tainted by accusations of data dredging, confounding, and bias.7 For example, observational studies showed lower rates of ischaemic heart disease among women using hormone replacement therapy, and these data were interpreted as advocating hormone replacement for healthy women, women with established ischaemic heart disease, and women with risk factors for ischaemic heart disease.8 However, randomised controlled trials showed that hormone replacement therapy actually increased the risk of ischaemic heart disease,9 indicating that the apparent protective effects seen in observational studies were due to bias. Cases such as this one show that medical interventions based solely on observational data should be carefully scrutinised, and the parachute is no exception.
Natural history of gravitational challenge
The effectiveness of an intervention has to be judged relative to non-intervention. Understanding the natural history of free fall is therefore imperative. If failure to use a parachute were associated with 100% mortality then any survival associated with its use might be considered evidence of effectiveness. However, an adverse outcome after free fall is by no means inevitable. Survival has been reported after gravitation challenges of more than 10 000 metres (33 000 feet).4 In addition, the use of parachutes is itself associated with morbidity and mortality.1-3 10 This is in part due to failure of the intervention. However, as with all interventions, parachutes are also associated with iatrogenic complications.3 Therefore, studies are required to calculate the balance of risks and benefits of parachute use.
The parachute and the healthy cohort effect
One of the major weaknesses of observational data is the possibility of bias, including selection bias and reporting bias, which can be obviated largely by using randomised controlled trials. The relevance to parachute use is that individuals jumping from aircraft without the help of a parachute are likely to have a high prevalence of pre-existing psychiatric morbidity. Individuals who use parachutes are likely to have less psychiatric morbidity and may also differ in key demographic factors, such as income and cigarette use. It follows, therefore, that the apparent protective effect of parachutes may be merely an example of the “healthy cohort” effect. Observational studies typically use multivariate analytical approaches, using maximum likelihood based modelling methods to try to adjust estimates of relative risk for these biases. Distasteful as these statistical adjustments are for the cognoscenti of evidence based medicine, no such analyses exist for assessing the presumed effects of the parachute.
The medicalisation of free fall
It is often said that doctors are interfering monsters obsessed with disease and power, who will not be satisfied until they control every aspect of our lives (Journal of Social Science, pick a volume). It might be argued that the pressure exerted on individuals to use parachutes is yet another example of a natural, life enhancing experience being turned into a situation of fear and dependency. The widespread use of the parachute may just be another example of doctors’ obsession with disease prevention and their misplaced belief in unproved technology to provide effective protection against occasional adverse events.
| What is already known about this topic
Parachutes are widely used to prevent death and major injury after gravitational challenge
Parachute use is associated with adverse effects due to failure of the intervention and iatrogenic injury
Studies of free fall do not show 100% mortality
What this study adds
No randomised controlled trials of parachute use have been undertaken
The basis for parachute use is purely observational, and its apparent efficacy could potentially be explained by a “healthy cohort” effect
Individuals who insist that all interventions need to be validated by a randomised controlled trial need to come down to earth with a bump
|
|
Parachutes and the military industrial complex
However sinister doctors may be, there are powers at large that are even more evil. The parachute industry has earned billions of dollars for vast multinational corporations whose profits depend on belief in the efficacy of their product. One would hardly expect these vast commercial concerns to have the bravery to test their product in the setting of a randomised controlled trial. Moreover, industry sponsored trials are more likely to conclude in favour of their commercial product,11 and it is unclear whether the results of such industry sponsored trials are reliable.
A call to (broken) arms
Only two options exist. The first is that we accept that, under exceptional circumstances, common sense might be applied when considering the potential risks and benefits of interventions. The second is that we continue our quest for the holy grail of exclusively evidence based interventions and preclude parachute use outside the context of a properly conducted trial. The dependency we have created in our population may make recruitment of the unenlightened masses to such a trial difficult. If so, we feel assured that those who advocate evidence based medicine and criticise use of interventions that lack an evidence base will not hesitate to demonstrate their commitment by volunteering for a double blind, randomised, placebo controlled, crossover trial.
Contributors: GCSS had the original idea. JPP tried to talk him out of it. JPP did the first literature search but GCSS lost it. GCSS drafted the manuscript but JPP deleted all the best jokes. GCSS is the guarantor, and JPP says it serves him right.
Funding: None.
Competing interests: None declared.
Ethical approval: Not required.
References
Belmont PJ Jr, Taylor KF, Mason KT, Shawen SB, Polly DW Jr, Klemme WR. Incidence, epidemiology, and occupational outcomes of thoracolumbar fractures among US Army aviators. J Trauma 2001;50: 855-61.[Web of Science][Medline]
Bricknell MC, Craig SC. Military parachuting injuries: a literature review. Occup Med (Lond) 1999;49: 17-26.
Lasczkowski G, Hasenfuss S, Verhoff M, Weiler G. An unusual airplane crash—deadly life saver. Unintentional activation of an automated reserve opening device causing airplane accident. Forensic Sci Int 2002;125: 250-3.[CrossRef][Web of Science][Medline]
Highest fall survived without a parachute. In: Cunningham A. Guinness world records 2002. London: Guinness World Records, 2002.
Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF, for the QUOROM Group. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Lancet 1999;354: 1896-1900.[CrossRef][Web of Science][Medline]
Lossius HM, Langhelle A, Reide E, Pillgram-Larsen J, Lossius TA, Laake P, et al. Reporting data following major trauma and analysing factors associated with outcome using the new Utstein style recommendations. Resuscitation 2001;50: 263-72.[CrossRef][Web of Science][Medline]
Davey Smith G, Ebrahim S. Data dredging, bias, or confounding. BMJ 2002;325: 1437-8.[Free Full Text]
Pines A, Mijatovic V, van der Mooren MJ, Kenemans P. Hormone replacement therapy and cardioprotection: basic concepts and clinical considerations. Eur J Obstet Gynecol Reprod Biol 1997;71: 193-7.[CrossRef][Web of Science][Medline]
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA 2002;288: 321-33.[Abstract/Free Full Text]
Lee CT, Williams P, Hadden WA. Parachuting for charity: is it worth the money? A 5-year audit of parachute injuries in Tayside and the cost to the NHS. Injury 1999;30: 283-7.[CrossRef][Web of Science][Medline]
Lexchin J, Bero LA, Djulbegovic B, Clark O. Pharmaceutical industry sponsorship and research outcome and quality: systematic review. BMJ 2003;326: 1167-70.[Abstract/Free Full Text]
Relevant Article
- Parachute approach to evidence based medicine
- Malcolm Potts, Ndola Prata, Julia Walsh, and Amy Grossman
BMJ 2006 333: 701-703. [Full Text] [PDF]
This article has been cited by other articles:
- Schmieder, R. E. (2009). Hypertension and Diabetes: What are the pros to treating early surrogates?. Diabetes Care 32: S294-S297 [Full text]
- Newman, T. B. (2009). Universal Bilirubin Screening, Guidelines, and Evidence. Pediatrics 124: 1199-1202 [Full text]
- Torres-Russotto, D., Landau, W. M., Harding, G. W., Bohne, B. A., Sun, K., Sinatra, P. M. (2009). Calibrated finger rub auditory screening test (CALFRAST). Neurology 72: 1595-1600 [Abstract] [Full text]
- Howick, J., Glasziou, P., Aronson, J. K (2009). The evolution of evidence hierarchies: what can Bradford Hill’s ‘guidelines for causation’ contribute?. JRSM 102: 186-194 [Full text]
- Ernst, A., Simoff, M., Ost, D., Herth, F. (2009). Response. Chest 135: 1402-1403 [Full text]
- Lauer, M. S. (2009). Discarding Logic: 2008 Ancel Keys Memorial Lecture. Circulation 119: 1533-1537 [Full text]
- Healy, D. (2009). Trussed in Evidence? Ambiguities at the Interface between Clinical Evidence and Clinical Practice. Transcultural Psychiatry 46: 16-37 [Abstract]
- Treasure, T. (2009). Are randomised trials needed in the era of rapidly evolving technologies?. Eur. J. Cardiothorac. Surg. 35: 474-478 [Abstract] [Full text]
- Dichtwald, S., Matot, I., Einav, S. (2009). Improving the Outcome of In-Hospital Cardiac Arrest: The Importance of Being EARNEST. SEMIN CARDIOTHORAC VASC ANESTH 13: 19-30 [Abstract]
- Grimes, D. A. (2009). Where Is the Evidence That the Resurgence of Nomograms Is Harmful?. ANN INTERN MED 150: 282-282 [Full text]
- Danchin, N., Chemla, D. (2009). Challenging doctors’ lifelong habits may be good for their patients: oxygen therapy in acute myocardial infarction. Heart 95: 176-177 [Full text]
- Mascola, A. J. (2008). Guided Mentorship in Evidence-Based Medicine for Psychiatry: A Pilot Cohort Study Supporting a Promising Method of Real-Time Clinical Instruction. Acad. Psychiatry 32: 475-483 [Abstract] [Full text]
- Matthews, D. R, Tsapas, A., Tsapas, A. (2008). Four decades of uncertainty: landmark trials in glycaemic control and cardiovascular outcome in type 2 diabetes. Diabetes and Vascular Disease Research 5: 216-218
- Sherman, E. M. S., Connolly, M. B., Slick, D. J., Eyrl, K. L., Steinbok, P., Farrell, K. (2008). Quality of Life and Seizure Outcome After Vagus Nerve Stimulation in Children With Intractable Epilepsy. J Child Neurol 23: 991-998 [Abstract]
- Logue, E. H. (2008). Geffen Faculty Highlight Concerns Linking CAIM and Conventional Researchers at UCLA Symposium. Evid Based Complement Alternat Med 0: nen051v2-nen051 [Abstract] [Full text]
- Professor the Lord Darzi of Denham, (2008). Evidence-based medicine and the NHS: a commentary. JRSM 101: 342-344 [Full text]
- Wachter, R. M., Flanders, S. A., Fee, C., Pronovost, P. J. (2008). Public Reporting of Antibiotic Timing in Patients with Pneumonia: Lessons from a Flawed Performance Measure. ANN INTERN MED 149: 29-32 [Abstract] [Full text]
- Bates, D. W (2008). Mountains in the clouds: patient safety research. Qual Saf Health Care 17: 156-157 [Full text]
- Tepper, J. E. (2008). Protons and Parachutes. JCO 26: 2436-2437 [Full text]
- Pronovost, P. J., Goeschel, C. A., Wachter, R. M. (2008). The Wisdom and Justice of Not Paying for “Preventable Complications”. JAMA 299: 2197-2199 [Full text]
- Devereaux, A., Christian, M. D., Dichter, J. R., Geiling, J. A., Rubinson, L. (2008). Summary of Suggestions From the Task Force for Mass Critical Care Summit, January 26-27, 2007. Chest 133: 1S-7S [Full text]
- Jordan, S. E., Armon, C., Argoff, C. E., Samuels, J., Backonja, M.-M. (2007). ASSESSMENT: USE OF EPIDURAL STEROID INJECTIONS TO TREAT RADICULAR LUMBOSACRAL PAIN: REPORT OF THE THERAPEUTICS AND TECHNOLOGY ASSESSMENT SUBCOMMITTEE OF THE AMERICAN ACADEMY OF NEUROLOGY. Neurology 69: 1191-1192 [Full text]
- Lighthall, G. K., Barr, J. (2007). The Use of Clinical Simulation Systems to Train Critical Care Physicians. J Intensive Care Med 22: 257-269 [Abstract]
- Auerbach, A. D., Landefeld, C. S., Shojania, K. G. (2007). The Tension between Needing to Improve Care and Knowing How to Do It. NEJM 357: 608-613 [Full text]
- McCartney, C. J. L., Wildsmith, J. A. W., Cornforth, B. M., Hargreaves, D. M., van Velzen, C., Hopkins, P. M. (2007). Ultrasound guidance for regional anaesthesia.. Br J Anaesth 99: 139-140 [Full text]
- Boutron, I., Ravaud, P., Nizard, R. (2007). The design and assessment of prospective randomised, controlled trials in orthopaedic surgery. J Bone Joint Surg Br 89-B: 858-863 [Abstract] [Full text]
- Wise, R. A. (2007). Ethical Issues Confronted In Pulmonary Clinical Trials. Proc Am Thorac Soc 4: 200-205 [Abstract] [Full text]
- Francisco, V. T., Butterfoss, F. D. (2007). Social Validation of Goals, Procedures, and Effects in Public Health. Health Promot Pract 8: 128-133 [Abstract]
- Nissenson, A. R. (2007). Influence of Industry on Renal Guideline Development Commentary: Keeping Our Eye on the Ball and Improving Chronic Kidney Disease Patient Outcomes. CJASN 2: 205-206 [Full text]
- Tan, C., Treasure, T., Browne, J., Utley, M., Davies, C. W H, Hemingway, H. (2007). Seeking consensus by formal methods: a health warning. JRSM 100: 10-14 [Full text]
- Treasure, T. (2006). The evidence on which to base practice: different tools for different times. Eur. J. Cardiothorac. Surg. 30: 819-824 [Full text]
- Hayward, R. A., Hofer, T. P., Vijan, S. (2006). Narrative review: lack of evidence for recommended low-density lipoprotein treatment targets: a solvable problem.. ANN INTERN MED 145: 520-530 [Abstract] [Full text]
- Potts, M., Prata, N., Walsh, J., Grossman, A. (2006). Parachute approach to evidence based medicine.. BMJ 333: 701-703 [Full text]
- Genuis, S. J. (2006). Health issues and the environment–an emerging paradigm for providers of obstetrical and gynaecological health care. Hum Reprod 21: 2201-2208 [Abstract] [Full text]
- Donnan, G. A., Davis, S. M., Schellinger, P. D., Hacke, W. (2006). Intra-Arterial Thrombolysis Is the Treatment of Choice for Basilar Thrombosis: Pro. Stroke 37: 2436-2437 [Full text]
- Sederer, L. I. (2006). The Evidence-Based Practice: Methods, Models, and Tools for Mental Health Professionals. Psychiatr. Serv. 57: 1219-1220 [Full text]
- Halamka, J. D. (2006). Health Information Technology: Shall We Wait for the Evidence?. ANN INTERN MED 144: 775-776 [Full text]
- Horan, F. T. (2005). Judging the evidence. J Bone Joint Surg Br 87-B: 1589-1590 [Full text]
- Claus, T., Schmitt, R., Stabroth, C., Luft, F. C., Kettritz, R., Gross, C. M. (2005). Where do we stand with renovascular hypertension?. Nephrol Dial Transplant 20: 1495-1498 [Full text]
- Marshall, A. C., Lock, J. E. (2005). Leaving Neverland: A Randomized Trial for Coarctation Shows Pediatric Interventional Cardiology Is Growing Up. Circulation 111: 3347-3348 [Full text]
- David, T. J (2005). Child abuse and paediatrics. JRSM 98: 229-231 [Full text]
- Schroeter, K. (2005). Stones From a Glass House: In Reply. Pediatrics 115: 1116-1117 [Full text]
- Lau, T., Carlsson, P.-O., Leung, P.S., Wolfrum, C., Asilmaz, E., Luca, E., Friedman, J.M., Stoffel, M., Verhave, J.C., Hillege, H.L., Burgerhof, J.G.M., Janssen, W.M.T., Gansevoort, R.T., Navis, G.J., de Zeeuw, D., de Jong, P.E., for the PREVEND Study Group, (2005). Why Less Diabetes with Blockade of the Renin-Angiotensin System?: Evidence for a Local Angiotensin-Generating System and Dose-Dependent Inhibition of Glucose-Stimulated Insulin Release by Angiotensin II in Isolated Pancreatic Islets. Diabetologia 47: 240-248, 2004. J. Am. Soc. Nephrol. 16: 567-573 [Full text]
- Sankar, R. (2004). Initial treatment of epilepsy with antiepileptic drugs: Pediatric issues. Neurology 63: S30-S39 [Abstract] [Full text]
- Christenfeld, N. J. S., Sloan, R. P., Carroll, D., Greenland, S. (2004). Risk Factors, Confounding, and the Illusion of Statistical Control. Psychosom. Med. 66: 868-875 [Abstract] [Full text]
- Doust, J., Del Mar, C. (2004). Why do doctors use treatments that do not work?. BMJ 328: 474-475 [Full text]
- (2004). Common Sense vs. Evidence-Based Medicine: Lessons from the Parachute. JWatch Emergency Med. 2004: 10-10 [Full text]